Mapping the Human Heart
- BY KRISTA DOSSETTI
- PHOTOGRAPHY BY JESSE CANTLEY
- November 7, 2016
Jamie Mackie is not a doctor. He never went to medical school and his salary is paltry compared to a surgeon’s. Nevertheless, he spends a 60-hour workweek in scrubs, logging in and out of operating rooms across the United States, outfitted something like an air traffic controller: He wears a headset and microphone while building an atlas of neon veins on the computer screen before him — only a thin lead window separating him from a cardiac surgeon tapping into a femoral artery on the other side.
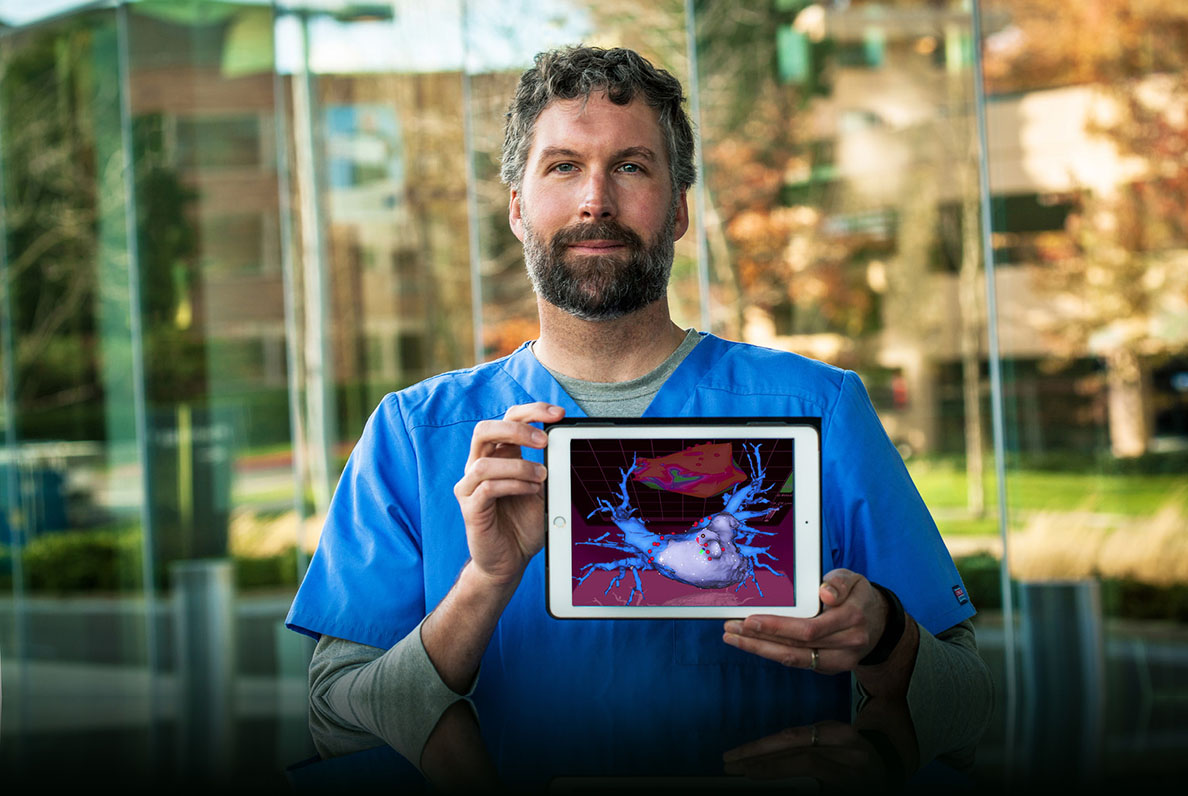
No, Jamie Mackie (MS ’13, Kinesiology) is not a doctor. He is the voice guiding them; the hands at the keyboard behind a growing medical technology that creates 3D, real-time, electro-anatomical maps of the cardiac system so surgeons can burn scars into precise locations in the human heart. Through a series of catheters and a 3D-mapping system made by the company he works for (Biosense Webster, a subsidiary of Johnson & Johnson), Mackie creates images of the heart for use during surgery that pinpoint any electrical impulses causing irregularities (arrhythmias) so they can be permanently fixed through cardiac ablation.
“I would say it’s a very new field of medicine,” Mackie explains. “There was no previous way to work inside the heart [like this], to the point that when you come across someone [about] who you would say, ‘That person’s been doing it a long time,’ we’re talking about eight years or so. I run into doctors in their 60s who have been doing this for 20 years that remember a time at the beginning of their careers when they were hooking up electrodes to car batteries and using DC current to burn structures inside of people’s hearts.”
“There’s this whole group of people who could have a better life without being on drugs — who could possibly have a cure instead of a treatment.”
Admittedly, he’s still a novice when it comes to creating the maps, having been hired by Biosense Webster just a year ago. Currently, he’s in training, which entails a breakneck travel schedule (his home base is Portland, Oregon) while shadowing technicians at hospitals and research centers throughout the country. By the end of the year, Mackie estimates, he’ll be ready to handle live surgeries on his own — a responsibility he doesn’t take lightly.
“I love the true health care aspect of this,” he says. “There’s this whole group of people who could have a better life without being on drugs — who could possibly have a cure instead of a treatment. My experience at East Bay was that you have to be able to work with all different types of people from different types of backgrounds. You can’t just sit behind the computer screen and not have empathy for the patient and not want to help the doctor. You have to think bigger than the small world you’re operating in.”
After graduating from Cal State East Bay’s master’s in kinesiology program, Mackie applied to the Arrhythmia Technology Institute (ATI), a cardiac device training center. It was there that he began learning how to create anatomical models of the heart using a variety of imaging tools such as fluoroscope, ultrasound, MRI, TTE (transthoracic echocardiogram) and CT (computerized tomography). From ATI, Mackie reports he was among the first group of students in his class to be placed with a biomedical company. “Because I had the background in physiology and anatomy [from my kinesiology studies] and had taken this interest in medical devices, it opened up this job opportunity,” he says.
Professor Becky Beal, one of two Cal State East Bay professors Mackie identifies as a personal mentor, sees the medical field as a natural fit for him — a role she says is unusual compared to the number of CSUEB graduates who go on to become physical or occupational therapists.
“Whenever you’re dealing with human care, [Cal State East Bay teaches students to] come at it from a multidisciplinary perspective, so it’s not just the technical, mechanical workings of a body — it’s also the context in which that occurs. [Jamie has] always been very smart about the context he’s working in, the clients, the emotional situation. He’s a very compassionate person, and sharp — he can talk to anybody. He put this together.”
Likewise, Professor Cathy Inouye, Mackie’s other CSUEB mentor, says the medical field is incredibly competitive. “Very few of our graduates move into cardiac rehab — it’s a difficult profession to enter and there’s a lot of additional education and certification that has to happen before you can get a position like that. I know he’ll be great at this because he’s very driven, he’s a powerful independent thinker, and he’s very calm.”
At least outwardly. “Right now, I spend a lot of time being nervous,” Mackie admits. “There’s a person under that blue tarp, and I need to be really, really good at this because every decision the doctor makes affects that patient, and I’m feeding the doctor information — I have to be the second-smartest person in the room. Little things make a big difference.”